
Spring 2023
QUERI Leadership: Setting the Course for 25 Years of Success and InnovationIn 1998, along with former Under Secretary for Health, Kenneth Kizer, MD, MPH, and former Director of VA’s Office of Research & Development (ORD), John Feussner, MD, the late John G. Demakis, MD, Director of HSR&D from 1998 to 2004, created the Quality Enhancement Research Initiative (QUERI) to advance the translation of evidence into practice – a novel notion at the time they authored “The Quality Enhancement Research Initiative: From Evidence to Action.” Three years earlier, VA initiated the largest structural healthcare transformation since it was established in 1946, which focused on two main goals: 1) to ensure predictable and consistent provision of high-quality healthcare throughout the system, and 2) to optimize the value of VA healthcare. Thus, QUERI’s original purpose was to use VA's health services research expertise and resources in an ongoing system-wide effort to improve the performance of the VA healthcare system and, thereby, optimize the quality of care for Veterans. Initially, QUERI focused on eight conditions that were highly prevalent among Veterans, including Chronic Heart Failure (CHF), Diabetes Mellitus (DM), Ischemic Heart Disease, HIV/AIDS, Mental Health, Spinal Cord Injury, Stroke, and Substance Use Disorder (SUD), soon after adding Colorectal Cancer and Polytrauma. These QUERI Centers were located across the United States and received guidance and direction from the QUERI National Advisory Council and a Research and Methodology Review Committee. In addition, each QUERI Center had an executive committee, comprised of approximately 15 VA and non-VA clinicians and researchers with expertise in the center’s clinical area, and each followed a standard six-step process:
QUERI Centers quickly began to release their research findings on quality and performance gaps and disseminate quality enhancement research tools and resources. For example, CHF QUERI implemented a multi-faceted intervention to improve outcomes among Veterans with chronic heart failure, and to reduce length-of-stay and readmission rates via the use of coordinated case management, patient education, and related strategies. Initial results included a significant decrease in 14-day readmission rates (from 14% to 5%) and increased patient stability upon discharge. DM QUERI increased provider awareness of the importance of blood pressure control, and their work led to significant improvements in the control of blood pressure, lipids, and HbA1c among Veterans with diabetes. Initial projections from these findings suggested VHA-wide reductions of 16,000 cardiovascular events and 11,500 deaths over a 20-year period (McQueen, Mittman, and Demakis, 2004). As associate director for QUERI, Lynn McQueen, DrPH, MS, RN, currently a performance officer at the Department of Health and Human Services, continued to grow QUERI by bringing in new investigators. Dr. McQueen also began collaborating with experts in the field of implementation, such as Brian Mittman, PhD, to better understand how to operationalize links between research and practice – and to systematically enhance the uptake of evidence-based practices (EBPs) in routine clinical functions. QUERI Centers helped identify specific barriers to involvement and critical organizational issues. This required closer collaborations between research, quality improvement, and clinical leadership. QUERI’s implementation efforts “up-ended” the traditional relationship of the health services researcher to the healthcare system. Over the 10 years since QUERI had begun, its focus had grown beyond “research as usual” to implementation science-focused projects with direct and immediate meaning for current practice and long-term quality improvement (Stetler et al., 2008). Currently a senior research scientist at Kaiser Permanente, Dr. Mittman served as QUERI Director from 2002 to 2004; he also served as its ambassador to the world of implementation science. As founding co-Editor-in-Chief of Implementation Science, Dr. Mittman was at the forefront of implementation science from the beginning. Establishing QUERI’s Center to Support Implementation Research and Practice (CIPRS), he helped guide researchers as they sought to discover methods and strategies that would facilitate the uptake of research into clinical practice. Joe Francis, MD, MPH, currently Executive Director of Analytics and Performance Integration in VA’s Office of Quality and Patient Safety (QPS), was Director of QUERI from 2004 to 2007. Dr. Francis strengthened QUERI’s ties to its VA operational partners, such as VA’s Office of Health Information and the Office of Patient Care Services. Leveraging academic partners supported by the Agency for Healthcare Research and Quality (AHRQ), he also initiated the Evidence Synthesis Program (ESP) to produce high-quality evidence syntheses for clinicians, managers, and policymakers. Further, he pushed for a more prominent role for health information technology (HIT) within QUERI. HIT provided data and information to facilitate implementation research, while implementation research helped to further HIT development. QUERI Centers collaborated with researchers, policymakers, practitioners, and administrators on HIT issues (Hynes et al., 2010). The key to working with numbers is to find ways to combine tools that center around evidence – What does the evidence say we should be doing or implementing? – with tools based on process observation and process improvement. —Joe Francis, MD Before becoming Director of HSR&D, David Atkins, MD, MPH, was Director of QUERI from 2008 to 2012. Dr. Atkins expanded the Evidence Synthesis Program (ESP) and increased clinical partnerships through creating Partnered Evaluation Centers, which used a mixture of QUERI and partner funding to support evaluation needs for clinical programs. Furthermore, he strengthened the program by identifying and working to address key challenges for QUERI and more broadly implementation research:
Dr. Atkins successfully ushered QUERI through its adolescence into adulthood, where it “developed a distinct identity from its ‘parent’ – health services research. Reaching adulthood is only the beginning of a lifelong process filled with failures as well as successes. What is essential is that we continue to learn and move forward. For implementation science and for QUERI, the next decade looks to be one filled with exciting possibilities, new partnerships, increasing relevance, and real accomplishment. —David Atkins, MD, MPH As Director of QUERI, Amy Kilbourne, PhD, MPH, brought her expertise in implementation science, learning health systems, and translation of clinical quality improvement intervention findings into actionable policy and practice to the job. Over the last decade, Dr. Kilbourne has transformed QUERI from 10 disease-specific centers to a national network of more than 45 cross-cutting centers addressing a range of VHA clinical and policy priorities, including clinical care and organizational efficiency, employee experience, burnout, health equity, and virtual care. QUERI Centers and Programs 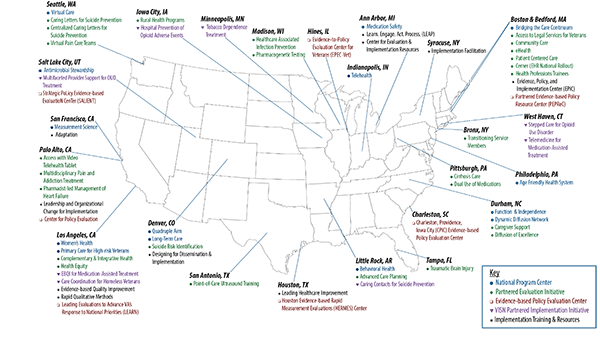
Under the leadership of Dr. Kilbourne and Deputy Director, Melissa Braganza, MPH, QUERI has fostered more than 100 partnerships with National Program Offices and VISNs to help make effective programs and policies work for Veterans and providers. They also built capacity to respond quickly to national and regional developments, expanded practical implementation and QI training and mentoring opportunities for VA employees, particularly for individuals with diverse backgrounds and experiences, and promoted an enterprise-wide approach to evidence development and evaluation. Notably, QUERI is helping to manage the recently established VHA Evidence-based Policy Subcommittee and supporting implementation of the Foundations for Evidence-Based Policymaking Act (Evidence Act) in VHA (Braganza et al., 2022). QUERI supports VA’s efforts to ensure healthcare programs and policies work for Veterans. Our funding comes from clinical operations. This means they have a say in what priorities we address in the rigorous implementation and evaluation of initiatives we support to help transform care for Veterans, their caregivers, families, and the workforce that cares for them. Our success is measured by making a difference in Veteran care. In turn, this is measured by how many providers deliver effective practices to their Veterans, whether Veterans’ health improves, and whether better programs and policies result from our work. —Amy Kilbourne, PhD, MPH QUERI continues to meet the changing needs of Veterans and the VA healthcare system in three ways. First, QUERI has evolved its approach from a pipeline model to the cyclical QUERI Implementation Roadmap, based on the Learning Health System Framework (Kilbourne et al., 2019). Second, QUERI continues to expand training opportunities to meet the growing demand for a diverse cadre of investigators and staff, trained in interdisciplinary fields, skilled at both research and operational nuances, and deft at tackling the complex system, environmental, and social factors to better shape the translation of science into real-world benefits for Veterans. Third, QUERI continues to pivot and adapt to rapid changes in technology and society, as well as emerging public health challenges.
Summary of the QUERI Implementation Roadmap Embracing new ideas and methods, especially from populations who have traditionally not been involved in healthcare research, will enable QUERI to continue fulfilling its mission of improving Veteran health and well-being through the alignment of science, implementation, and policy changes. Current QUERI Program Leadership
QUERI would also like to thank the following former QUERI program managers and staff for their dedication, expertise and contributions to help make QUERI the program it is today: Faith Booker, MPH; Jorge Caridad, BA; Linda McIvor, MHS; John Midolo, MPH; Kristina Nord, MSW; and Angela Whatley, PhD. |