Spring 2024
» Table of Contents
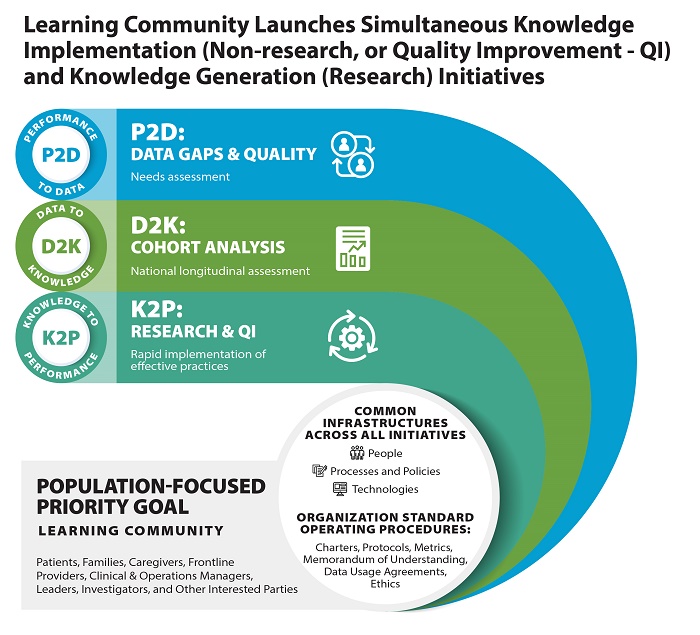
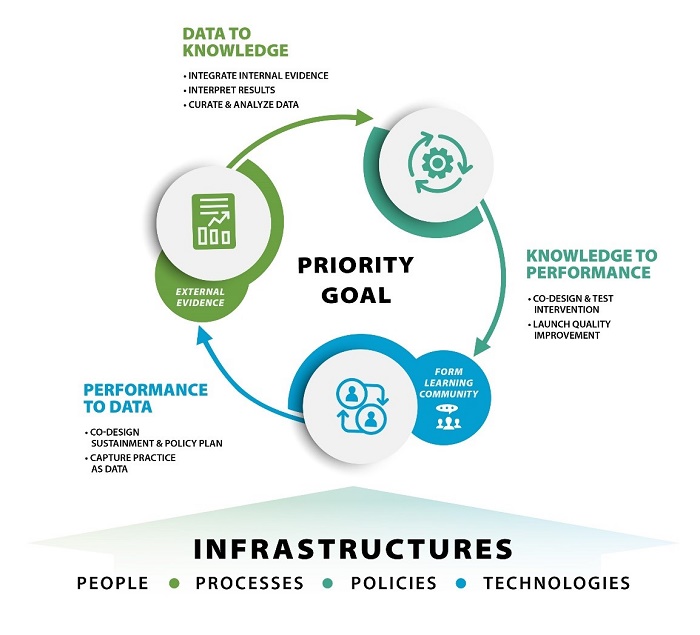
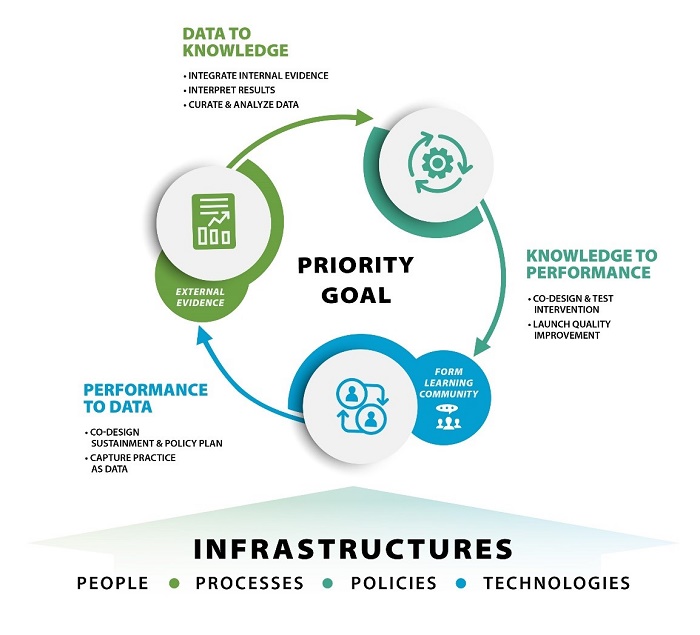
First defined by the Institute of Medicine in 2007, a learning health system involves a “system in which science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with (evidence-based) practices seamlessly embedded in the care process, patients and families as active participants in all elements, and new knowledge is captured as an integral by-product of the care experience.” These functions include formation of a learning community, which is a workgroup that is focused on achieving a shared health priority goal through ongoing generation and management of evidence-building and evaluation initiatives that rely on enterprise-wide sources of clinical, system, and population-based data and infrastructure. The infrastructure includes standard operating procedures based on organizational processes and policies for ongoing data curation and analysis that will support enterprise-wide evidence-generation and evaluation activities addressing the priority goal.
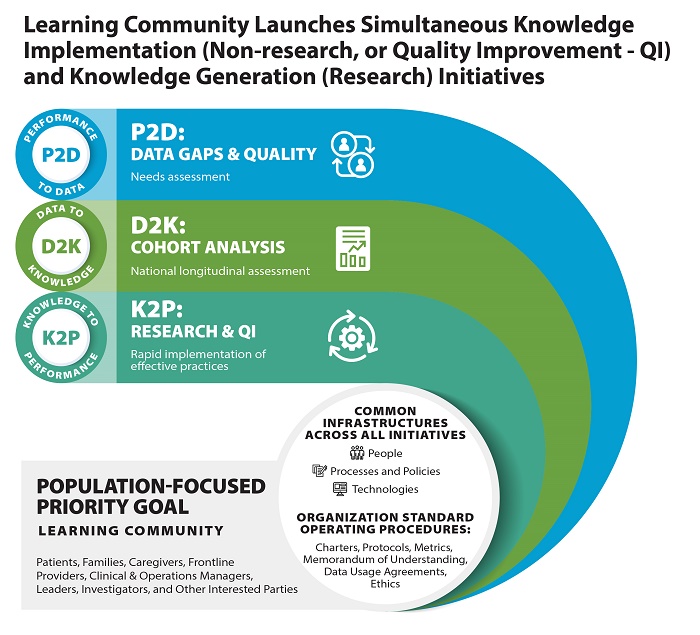
QUERI learning health systems follow a framework with milestones that must be completed during the startup award period and are aligned with the specific aims of the priority goal. Milestones include:
- Form learning community/subcommittee focused on the priority goal, develop a learning community charter, and finalize membership. Operationalize the shared priority goal into specific aims, metrics, and milestones to be accomplished each year. Identify the knowledge gaps and Veteran and provider-focused outcomes to be assessed.
- Identify the metrics and data sources to accomplish specific aims, including the population in which the evidence-building and evaluation activities will commence. Create standard operating procedures (SOPs) to optimize data curation, governance (including data stewardship processes), ethics (non-research) review/approvals, synthesis, and analysis of enterprise-wide, national data to support specific aims, including for large cohort studies, national evaluations, and quality improvement initiatives.
- Specify the steps to accomplish the specific aims to identify drivers of quality gaps, development of the cohort analysis, and implementation of the quality improvement intervention to rapidly assess and/or deploy new programs or policies. Describe how these steps will inform additional data and variables needed for the national cohort study to identify drivers of better Veteran and provider outcomes in order to inform enterprise-wide intervention studies.
- Launch the national data cohort study: create a combined data set that establishes the underlying cohort to inform the cohort study and multiple evidence-building and evaluation projects.
- Launch a quality improvement initiative that involves the rapid implementation of an effective practice or policy to inform scale-up and sustainment nationally.
- Analyze the data, develop publications/briefings, and refine the SOPs based on the needs assessment, cohort development, and quality improvement initiative.
- Assemble impacts based on the QUERI ACTION framework across the aims and apply a communication strategy to brief VA program office and national leadership, and communicate impacts to frontline providers, Veteran groups, investigators, and operational leaders.
- Identify opportunities for new initiatives, including future evidence-building activities (e.g., national intervention trial or cohort study), evaluation plans for VA Evidence Act submission, and/or quality improvement initiatives.
Geriatrics Learning Health System Milestones
Leads: Dawn Bravata, MD, and Cathy Schubert, MD
The Geriatrics Learning Health System (LHS) QUERI start-up addresses the QUERI goal of driving a culture of rapid learning for VA’s transformation to a high reliability organization and directly supports the VA priority goal of improving access to and quality of aging and long-term care support for Veterans including Veterans residing in rural areas. The overall objective of the LHS is to support community-dwelling older Veterans as they transition from the inpatient setting to home. The Geriatrics LHS aims to accomplish the following during the 18-month infrastructure start-up phase:
- Build and support a learning community that will consider the data infrastructure, evidence building, and program evaluation needs at three levels: Veterans and caregivers, VA facilities, and the VA enterprise. The learning community will also identify necessary personnel, processes, and policies to support the LHS objective of supporting community-dwelling older Veterans as they transition from hospital to home; establish listening/learning and communication/dissemination strategies; inform project designs; and develop future work plans.
- Establish a data core to develop and refine standard operating procedures (SOPs) and policies for ongoing data curation, governance, and analysis that will support leadership as they engage in strategic planning and policy evaluation, and quality improvement at the facility, VISN, and enterprise levels. The data core will also identify metrics and data sources for the planned LHS projects.
- Conduct a needs assessment to identify elements of successful transitions at high-performing sites and barriers to successful transitions at low-performing sites, and identify gaps in the existing VA data infrastructure (e.g., identify the Veteran, caregiver, and facility characteristics or outcomes that are not currently available, but that would inform policy or allow for program adoption or evaluation).
- Construct a cohort of community-dwelling older Veterans who have been discharged from a VA inpatient ward to the outpatient setting to compare the risk of 30-day readmissions between urban versus rural-dwelling Veterans.
- Evaluate the Coordinated Transitional Care (C-TraC) program implementation at 13 VA sites that are in various stages of implementation. C-TraC is a program that uses minimal resources to limit rehospitalizations while simultaneously empowering Veterans and their caregivers to better manage their healthcare after a hospitalization.
Homelessness Learning Health System (SHELTER) Milestones
MPIs: Audrey Jones, PhD, Richard Nelson, PhD, Jack Tsai, PhD
The Homelessness LHS will establish the Scientific approaches to improve Housing and Economic security outcomes advanced by a Learning health system Through data-driven Evaluation and Research (SHELTER) learning community. The goal of the SHELTER learning community is to guide policy to improve Veterans’ housing security and prevent and end Veteran homelessness through enhanced VA homelessness data infrastructure. This learning community will be comprised of experts in homelessness and VA and non-VA homelessness data systems that will consider the data infrastructure and program evaluation needs of homeless Veterans and the VA Homeless Program Office (HPO). SHELTER will:
- Conduct a needs assessment to determine gaps in data availability and quality. Specifically, SHELTER will conduct an environmental scan of published reports and metadata. This will be done through a systematic search of research and quality improvement publications, VA operational reports and websites, and metadata describing VA data systems to identify measures of homelessness and housing instability.
- Perform qualitative interviews to obtain stakeholder perspectives of data needs. SHELTER will recruit leaders from the HPO and other federal agencies, VA front-line staff, and researchers and elicit from them data sources that would improve their ability to perform their jobs.
- Using existing data systems, SHELTER will assemble a dataset that can track Veterans’ housing status, clinical characteristics, and other social determinants of health over time. The data sources for this exercise will consist of those known to the team from previous work as well as new sources identified through the environmental scan and qualitative interviews. Housing status will be obtained through structured and unstructured elements from these data sources.
- With this dataset, SHELTER will construct a cohort of Veterans experiencing homelessness or risk of homelessness that tracks housing status longitudinally. Once completed, this dataset will be a resource for future evaluations of VA housing-related initiatives.
- Collect prospective data on homeless experience, recurrence, and risk and protective factors from a subsample of previously contacted Veterans. The survey findings will provide information on the validity of SHELTER’s EHR-derived algorithms, provide new insights on the dynamics that contribute to returns to homelessness, and identify gaps and areas for improvement in existing data systems.
- Most assessments of Veterans’ experience in homelessness and evaluations of programs and policies to reduce or prevent Veteran homelessness are conducted using data from Veterans enrolled in the VA healthcare system. However, because many Veterans do not use VA as their primary source of healthcare, this approach to data capture provides an incomplete picture of Veterans’ housing status over time. Other data sources are necessary to build a comprehensive understanding of the Veteran life journey to inform programs and policies; one example is the Homelessness Management Information System (HMIS). Continuums of Care (CoCs) are required by the U.S. Department of Housing and Urban Development to collect client-level data and information on provision of housing and services to individuals and families experiencing homelessness in local HMIS systems. As a quality improvement project, SHELTER will develop a data exchange between the VA HPO and several CoCs to develop a data exchange with their Coordinated Entry Systems.
|