
Fall 2023
» Table of Contents
One of VA’s top priorities is to “connect Veterans to the soonest and best care.” To help address this priority, HSR/QUERI have launched several initiatives evaluating Veterans’ access, quality, and experience of VA and community care. HSR’s new COnsortia of REsearch (CORE), Access and Community Care Engagement Network Team (ACCENT), is expanding upon past work to help inform VA efforts to optimize Veteran access to care across in-person, virtual, and community care services.
The following are just a few of the evaluations led by HSR/QUERI investigators to examine community care as it affects Veterans’ healthcare and wellbeing.
VA versus Non-VA Quality of Care: A Systematic Review
HSR’s Evidence Synthesis Program (ESP) Center located at the VA Greater Los Angeles Healthcare System conducted a systematic review to compare quality and safety, access, patient experience, efficiency (cost), and equity between VA and non-VA care. As detailed in VA versus Non-VA Quality of Care: A Systematic Review (updated in April 2023), most published studies comparing VA and non-VA quality of care found that VA care is as good as, or better than, care in the community. This was the case for both surgical care and nonsurgical care – and for community care of Veterans and community care of non-Veterans. Results also showed that VA care is as good as, or better than, care in the community in regard to quality and safety.
Challenges of Community Providers Caring for Veterans in Rural Settings
One of 19 articles in a special issue of the Journal of General Internal Medicine (JGIM), Veterans’ Access to Care, reports on the challenges of non-VA primary care providers who care for Veterans. The article addresses three determinants of access: provider, health system, and community perspectives. Investigators interviewed clinicians and staff, identifying four themes and multiple challenges related to providing care for Veterans residing in rural settings: 1) Confusion, variability, and delays for VA administrative processes; 2) clarifying responsibility for dual-user Veteran care; 3) accessing and sharing medical records outside VA; and 4) negotiating communication pathways between systems and clinicians. Findings from this article suggest that clearer pathways of communication, streamlined or demystified administrative processes, access to records, and clarification of roles may help community care clinicians and staff care for Veterans living in rural settings.
Improving Care Coordination between VA and Community Settings
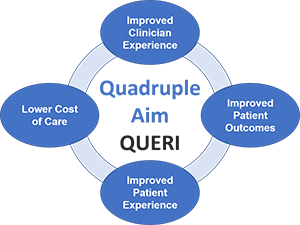 The Quadruple Aim QUERI Program aims to enhance Veteran outcomes and experiences, increase provider engagement, and reduce cost of care by providing value-based care coordination between VA and community settings. Veterans who receive care in both VA and community settings are at risk for fragmented, poorly coordinated care, which may contribute to adverse outcomes, poor experiences, and increased costs of care. In partnership with the VA Offices of Mental Health and Suicide Prevention, Nursing Services, Care Management and Social Work, Community Care, and VISN 19 (VA Rocky Mountain Network), QUERI investigators are working to transform Veteran care by implementing three effective practices that address major care coordination challenges: Whole Health Coaching in VA Pain Management Teams Initiative seeks to improve the care and experience of Veterans receiving chronic pain care in VA through integrating Whole Health Coaches on Pain Management Teams. Care Coordination Management provides integrated case management to ensure high-risk Veterans receive timely access to services and reduces adverse outcomes. Approximately 180 staff have been trained across six sites, to date. Transitions Nurse Program for Home Health Care (TNP-HHC) is designed to improve care for Veterans discharged with home healthcare services by providing evidence-based training and facilitation for nurses and/or social workers who implement this program at a VAMC. TNP-HHC Transitions Coordinators at San Diego VAMC, Shreveport Overton Brooks VAMC, and Lexington VAMC have served nearly 160 Veterans at 35 community, non-VA home health care agencies. The Quadruple Aim QUERI Program aims to enhance Veteran outcomes and experiences, increase provider engagement, and reduce cost of care by providing value-based care coordination between VA and community settings. Veterans who receive care in both VA and community settings are at risk for fragmented, poorly coordinated care, which may contribute to adverse outcomes, poor experiences, and increased costs of care. In partnership with the VA Offices of Mental Health and Suicide Prevention, Nursing Services, Care Management and Social Work, Community Care, and VISN 19 (VA Rocky Mountain Network), QUERI investigators are working to transform Veteran care by implementing three effective practices that address major care coordination challenges: Whole Health Coaching in VA Pain Management Teams Initiative seeks to improve the care and experience of Veterans receiving chronic pain care in VA through integrating Whole Health Coaches on Pain Management Teams. Care Coordination Management provides integrated case management to ensure high-risk Veterans receive timely access to services and reduces adverse outcomes. Approximately 180 staff have been trained across six sites, to date. Transitions Nurse Program for Home Health Care (TNP-HHC) is designed to improve care for Veterans discharged with home healthcare services by providing evidence-based training and facilitation for nurses and/or social workers who implement this program at a VAMC. TNP-HHC Transitions Coordinators at San Diego VAMC, Shreveport Overton Brooks VAMC, and Lexington VAMC have served nearly 160 Veterans at 35 community, non-VA home health care agencies.
Helping VA Implement Patient Safety Practices in Community Care
 In partnership with VA’s Office of Integrated Veteran Care (IVC) and the National Center for Patient Safety (NCPS), QUERI’s VA Implementation of Patient Safety Practices in Community Care (VIPS-CC) is evaluating the national implementation of the Patient Safety Guidebook to ensure safe, timely, and high-quality care for Veterans using community care. Beginning in late 2018, VA mandated implementation of safety processes using the Patient Safety Events in Community Care: Reporting, Investigation, and Improvement Guidebook. The Guidebook seeks to standardize community care (CC) safety event collection and reporting across VA and CC providers using the Joint Patient Safety Reporting System (JPSR). Ensuring effective implementation of these processes is critical as Veterans use of CC increases. VIPs-CC QUERI aims to help improve adoption and implementation of Guidebook processes by VA facilities. VIPS-CC works to: In partnership with VA’s Office of Integrated Veteran Care (IVC) and the National Center for Patient Safety (NCPS), QUERI’s VA Implementation of Patient Safety Practices in Community Care (VIPS-CC) is evaluating the national implementation of the Patient Safety Guidebook to ensure safe, timely, and high-quality care for Veterans using community care. Beginning in late 2018, VA mandated implementation of safety processes using the Patient Safety Events in Community Care: Reporting, Investigation, and Improvement Guidebook. The Guidebook seeks to standardize community care (CC) safety event collection and reporting across VA and CC providers using the Joint Patient Safety Reporting System (JPSR). Ensuring effective implementation of these processes is critical as Veterans use of CC increases. VIPs-CC QUERI aims to help improve adoption and implementation of Guidebook processes by VA facilities. VIPS-CC works to:
- Assess variation across VISNs and facilities in the implementation of standardized Guidebook processes used for patient safety reporting, investigation, and improvement.
- Examine organizational contextual factors (e.g., safety culture, leadership engagement) that influence implementation for sites with high vs. low fidelity to Guidebook safety processes.
- Describe variation across VISNs and sites in service outcomes.
- Identify specific combinations of implementation strategies and organizational factors that distinguish high- vs. low-performing sites on their implementation and service outcomes.
Partnered Evidence-based Policy Resource Center (PEPReC) Access to Care Evaluations
 PEPReC was established in 2017 to provide timely, rigorous data analysis to support the development of high-priority policy, planning, management initiatives and program evaluations. PEPReC partners with more than 10 National Program Offices to address policy priorities, including VA’s implementation of the MISSION Act, PACT Act, and Evidence Act. Below are just a few findings from PEPReC evaluations of community care. PEPReC was established in 2017 to provide timely, rigorous data analysis to support the development of high-priority policy, planning, management initiatives and program evaluations. PEPReC partners with more than 10 National Program Offices to address policy priorities, including VA’s implementation of the MISSION Act, PACT Act, and Evidence Act. Below are just a few findings from PEPReC evaluations of community care.
- Increasing emergency department (ED) physician capacity may decrease emergency care visits to the community and subsequent specialty care leakage from VA hospitals. Palani S, Garrido M, Tenso K, and Pizer S. Community care emergency room use and specialty care leakage from Veterans Health Administration hospitals. Academic Emergency Medicine. April 2023;30(4):379-387.
- Elective outpatient hernia surgery analyses that fail to account for the selection of higher risk patients to community care find poorer post-operative outcomes in non-VA surgeries. Mull H, Kabdiyeva A, Ndugga N, et al. What is the role of selection bias in quality comparisons between VHA and community care? Example of elective hernia surgery. Health Services Research. June 2023;58(3):654-662.
- PEPReC is currently examining how much of the increase in the use of the VA community care program is accounted for by Veterans shifting their service use from financing by Medicare or private insurance to VA community care. Rose L, Tran D, Wu S, et al. Payer shifting after expansions in access to private care among Veterans. Health Services Research. April 19, 2023; Online ahead of print.
Further, PEPReC is evaluating whether increasing VA emergency department capacity is cost-effective compared to purchasing emergency care from the community. These findings may help VA leadership in making decisions on minimizing care leakage to community and CC spending, since care leakage to the community can cause care coordination challenges, poor health outcomes, and can be a financial burden to VA in the long run. |
