
Fall 2023
» Table of Contents
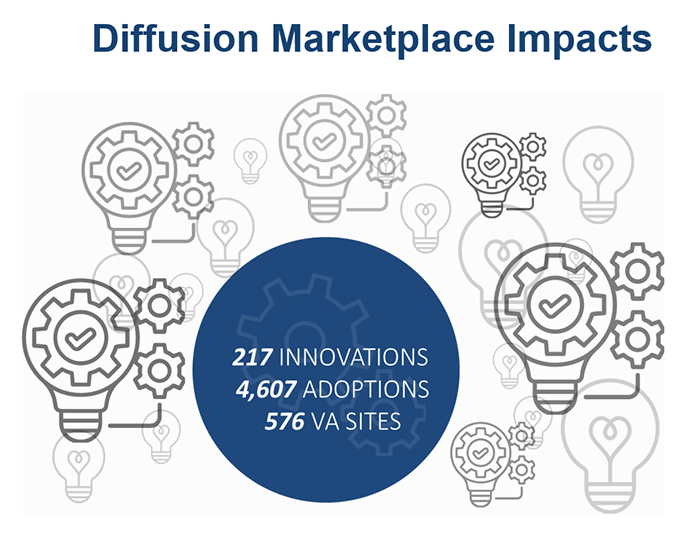
Since 2017, QUERI and the Innovation Ecosystem’s (VHA IE) Diffusion of Excellence have collaborated closely to scale-up, spread, and sustain evidence-informed practices and measure the multi-faceted impact of these efforts on Veterans and their families, VA employees, and the VA healthcare system.
The VHA Innovation Ecosystem leverages the collective power of innovation champions from across VA, academia, non-profit, and industry to operationalize innovation within the VA healthcare system to meet its goal of scaling up promising practices.
QUERI teams have developed methods and tools to promote the national implementation of 20 Diffusion Marketplace practices, including six National Diffusion Practices that have been prioritized for implementation across the VA healthcare system. The following are a few examples of these successes.
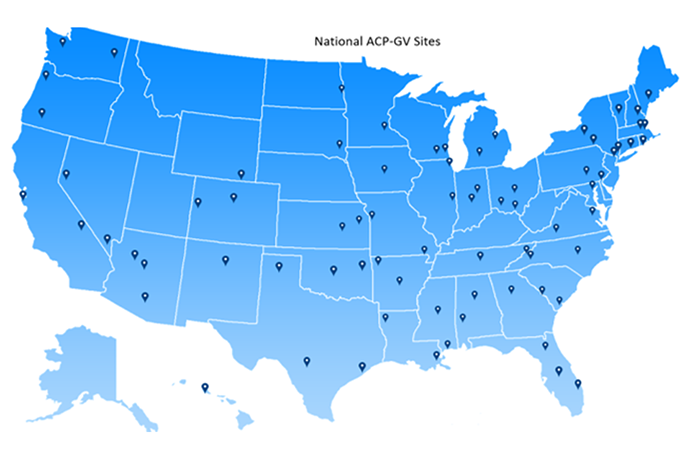
Advance Care Planning via Group Visits Prompt Veterans to Consider What Matters Most
Advance Care Planning via Group (ACP-GV) Visits engage Veterans and those they trust to make informed decisions about their future care, which is important given that an estimated 6.7 million Veterans enrolled in VA healthcare do not have an Advance Directive. ACP-GV engages Veterans, caregivers, and those they trust in advance care planning by facilitating a group discussion that elicits personal experience(s) and encourages participants to identify a ‘next step’ to take in the process of planning for future healthcare needs. Participants are encouraged to consider what matters most to them. Led by Dr. Monica Matthieu, this QUERI Partnered Evaluation Initiative has partnered with two national program offices and 18 VISNs to develop tools and strategies to promote this National Diffusion Practice across the VA healthcare system. Thus far, ACP-GV is being used by 955 providers across 75 facilities to serve nearly 28,000 Veterans.
Improving Prosthetic Care for Veterans with Major Limb Loss
FLOW3 is a novel workflow computerized management system that incorporates three custom-designed applications to facilitate the process for obtaining prosthetic limbs for Veterans – from prescription, specification, procurement, and fabrication to delivery and verification. This is important because VA provides care for more than 50,000 Veterans with major limb loss, including those with amputations secondary to combat. The FLOW3 system makes the prosthetic limb process more predictable and consistent, creating a high-quality experience for Veterans and staff. In order to implement this National Diffusion Practice across VA, the FLOW3 program collaborated with QUERI evaluators – led by Dr. Chelsea Leonard – to assess the practice in VISN 22 (VA Desert Pacific Healthcare Network) and VISN 9 (VA Mid-South Healthcare Network). FLOW3 has now been adopted at 157 facilities nationwide. Further, more than 30,000 complete prostheses or socket replacements for 17,621 unique Veterans have been prescribed using FLOW3.
Making Caregivers a Priority
 Caregivers FIRST is offered to caregivers of Veterans of all eras and diagnoses – and is a highly adaptable “grab and go” curriculum package that includes four in-person classes (60-75 minutes each) and optional training topics. Depending on the location, Caregiver Support Program teams at local VA facilities offer the group sessions either in-person or virtually. Every participant enrolled in Caregivers FIRST receives a workbook and supplemental materials that guide topics of interest, including coping with anger and other emotions, substance abuse, sleep challenges, and more. The program is designed to help caregivers build coping, support-seeking, and hands-on skills and strategies while connecting with available VA supports – and each other. The VA Caregiver Support Program and Function QUERI, which is led by Drs. Nicki Hastings, Courtney Van Houtven, and Kelli Allen, are working together to scale-up and spread Caregivers FIRST. To date, Caregivers FIRST has been implemented in 125 sites, reaching more than 3,200 family or friend caregivers of Veterans. Caregivers FIRST is offered to caregivers of Veterans of all eras and diagnoses – and is a highly adaptable “grab and go” curriculum package that includes four in-person classes (60-75 minutes each) and optional training topics. Depending on the location, Caregiver Support Program teams at local VA facilities offer the group sessions either in-person or virtually. Every participant enrolled in Caregivers FIRST receives a workbook and supplemental materials that guide topics of interest, including coping with anger and other emotions, substance abuse, sleep challenges, and more. The program is designed to help caregivers build coping, support-seeking, and hands-on skills and strategies while connecting with available VA supports – and each other. The VA Caregiver Support Program and Function QUERI, which is led by Drs. Nicki Hastings, Courtney Van Houtven, and Kelli Allen, are working together to scale-up and spread Caregivers FIRST. To date, Caregivers FIRST has been implemented in 125 sites, reaching more than 3,200 family or friend caregivers of Veterans.
STRIDE Walking Program Expands
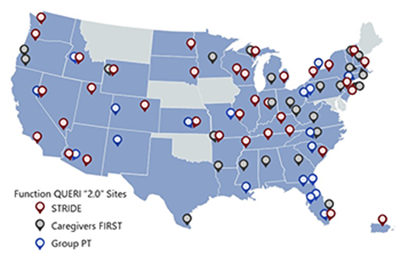 The STRIDE walking program aims to reduce preventable harm of hospital-associated disability. STRIDE features an early assessment, supervised ambulation, and patient education about the importance of daily walking – all designed to ensure patient safety during program participation. The Function QUERI STRIDE team received the 2022 National Diffusion Award and has supported the implementation of STRIDE in nearly 30 sites, training 879 providers, and serving 8,340 Veterans, to date. Function QUERI works to implement and evaluate effective practices to maximize function and independence in Veterans. Thus far, Function QUERI practices have been implemented in 130 VA medical centers across the country. The STRIDE walking program aims to reduce preventable harm of hospital-associated disability. STRIDE features an early assessment, supervised ambulation, and patient education about the importance of daily walking – all designed to ensure patient safety during program participation. The Function QUERI STRIDE team received the 2022 National Diffusion Award and has supported the implementation of STRIDE in nearly 30 sites, training 879 providers, and serving 8,340 Veterans, to date. Function QUERI works to implement and evaluate effective practices to maximize function and independence in Veterans. Thus far, Function QUERI practices have been implemented in 130 VA medical centers across the country.
I have had those patients where I knew they needed something like STRIDE, so there is great satisfaction in seeing visible progress with these patients going home a little stronger than they started… —Charleston VAMC Provider
Surgical Pause Practice Adopted as National Program
 Surgical Pause involves a pre-operative frailty screening for frail Veterans undergoing surgery so that their care plan can be optimized. More than 102,000 Veterans have been assessed using the Surgical Pause tool. Recently, VA’s National Surgery Office (NSO) announced that it will support the transition of the Surgical Pause Practice to an operational program. Based on the experience of pilot sites, this program could significantly reduce deaths related to surgery in frail, older Veterans. Led by Dr. Daniel Hall, the Surgical Pause Team has worked closely with the VHA Diffusion of Excellence to replicate this promising practice in more than 50 VA medical centers (VAMC) with positive results. SAGE QUERI uses the surgical pause to trigger formal goal clarification prior to surgery as one of four “Age Friendly” healthcare practices, and the PAUSE Trial at the Palo Alto, Houston, and Nashville VAMCs uses the Risk Analysis Index (RAI) to prompt consultation of a multidisciplinary clinic to optimize the perioperative planning for frail Veterans considering surgery. Surgical Pause involves a pre-operative frailty screening for frail Veterans undergoing surgery so that their care plan can be optimized. More than 102,000 Veterans have been assessed using the Surgical Pause tool. Recently, VA’s National Surgery Office (NSO) announced that it will support the transition of the Surgical Pause Practice to an operational program. Based on the experience of pilot sites, this program could significantly reduce deaths related to surgery in frail, older Veterans. Led by Dr. Daniel Hall, the Surgical Pause Team has worked closely with the VHA Diffusion of Excellence to replicate this promising practice in more than 50 VA medical centers (VAMC) with positive results. SAGE QUERI uses the surgical pause to trigger formal goal clarification prior to surgery as one of four “Age Friendly” healthcare practices, and the PAUSE Trial at the Palo Alto, Houston, and Nashville VAMCs uses the Risk Analysis Index (RAI) to prompt consultation of a multidisciplinary clinic to optimize the perioperative planning for frail Veterans considering surgery.
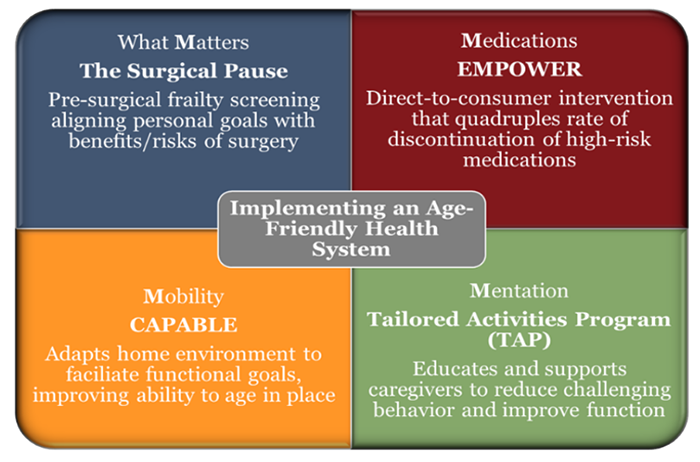
Improving Patient Safety by Deprescribing Inappropriate Medications
VIONE is a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. QUERI teams are providing evaluation support and training in LEAP (Learn. Engage. Act. Process.)—an evidence-based quality improvement (QI) strategy—to support the national implementation of VIONE. During LEAP, teams complete a QI project with the help of a coach and support from a learning community comprised of other teams. LEAP team members gain experience in applying QI methods within the demands of everyday clinical practice and develop the skills and knowledge to lead new QI initiatives to optimize care for their patients. VIONE has been adopted by 15,895 providers across 133 VA facilities, reaching 694,826 Veterans. Led by Drs. Jeremy Sussman and Laura Damschroder, LEAP is available on VA’s Online Marketplace.
 I would definitely recommend LEAP to others because it provides a strong foundation for setting up quality improvement projects. It really helps guide you step-by-step through the process, and the skills you develop are transferrable to other research, quality improvement projects or skills in our clinical practice. —VIONE LEAP Participant I would definitely recommend LEAP to others because it provides a strong foundation for setting up quality improvement projects. It really helps guide you step-by-step through the process, and the skills you develop are transferrable to other research, quality improvement projects or skills in our clinical practice. —VIONE LEAP Participant
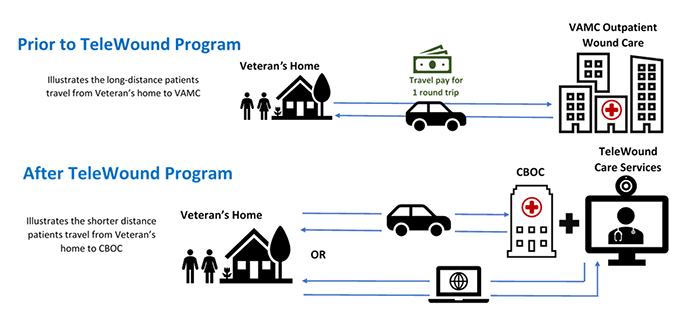
The TeleWound Practice Partnered Evaluation Initiative works to assess the impact of TeleWound Practice on clinical and healthcare system outcomes, helping to provide optimal wound care for Veterans, particularly those that live a greater distance from a VA facility. The TeleWound Practice Program provides wound care to Veterans using telehealth technologies – and was selected for regional-level roll-out by VA’s Undersecretary for Health as part of the Diffusion of Excellence Shark Tank competition. Veterans who received TeleWound care at VISN 15 implementation sites saved an average of 303 miles in travel with a cost savings of $170.
Once a week I’ll take a picture of my wound and send it in. They can look at it and say, ‘Oh yeah, it looks like it’s doing this or do we want to do that.’ It’s more interactive in the wound care itself. It gets the patient more involved with wound care than [leaving] everything to the doctor. —Veteran who received TeleWound care
Providing Broader Evaluation Support to the Innovation Ecosystem
 In addition to promoting the uptake of specific Diffusion Marketplace practices, QUERI teams are providing broader evaluation support to the Innovation Ecosystem, including conducting rigorous mixed-methods evaluations of the overall Diffusion of Excellence and Innovators Network programs – and developing products to enhance the impact of these programs. For example, the Spreading Healthcare Access, Activities, Research and Knowledge (SHAARK) QUERI Partnered Evaluation developed the QuickView and Wishlist decision support tools to help VA leaders compare Shark Tank practices and make informed decisions on local need, implementation resources, and practice fit. In addition to promoting the uptake of specific Diffusion Marketplace practices, QUERI teams are providing broader evaluation support to the Innovation Ecosystem, including conducting rigorous mixed-methods evaluations of the overall Diffusion of Excellence and Innovators Network programs – and developing products to enhance the impact of these programs. For example, the Spreading Healthcare Access, Activities, Research and Knowledge (SHAARK) QUERI Partnered Evaluation developed the QuickView and Wishlist decision support tools to help VA leaders compare Shark Tank practices and make informed decisions on local need, implementation resources, and practice fit.
Diffusion of Excellence Shark Tank Impacts
- 99% VHA parent health systems/facilities submitted 3,281 applications
- 88 Promising Practices
- 1,440+ Adoptions of Promising Practices
- 56% Facilities sustaining Promising Practices
 Led by Dr. Nicholas Bowersox, QUERI’s Center for Evaluation and Implementation Resources (CEIR) has helped coordinate the subject matter expert review and rating of nearly 500 Shark Tank semi-finalist innovations. CEIR also provided targeted feedback and strategic planning support to 83 Promising Practice and National Diffusion Practice teams. Led by Dr. Nicholas Bowersox, QUERI’s Center for Evaluation and Implementation Resources (CEIR) has helped coordinate the subject matter expert review and rating of nearly 500 Shark Tank semi-finalist innovations. CEIR also provided targeted feedback and strategic planning support to 83 Promising Practice and National Diffusion Practice teams.
|
